Modern PD* -
Patients are safer from nosocomial infections when dialyzing at home1
*Modern PD is the culmination of multiple recent advancements in clinical practice and innovations in technology that, in combination, are yielding improved survival, increasing patient satisfaction and clinical outcomes that in some cases are outpacing those of HD
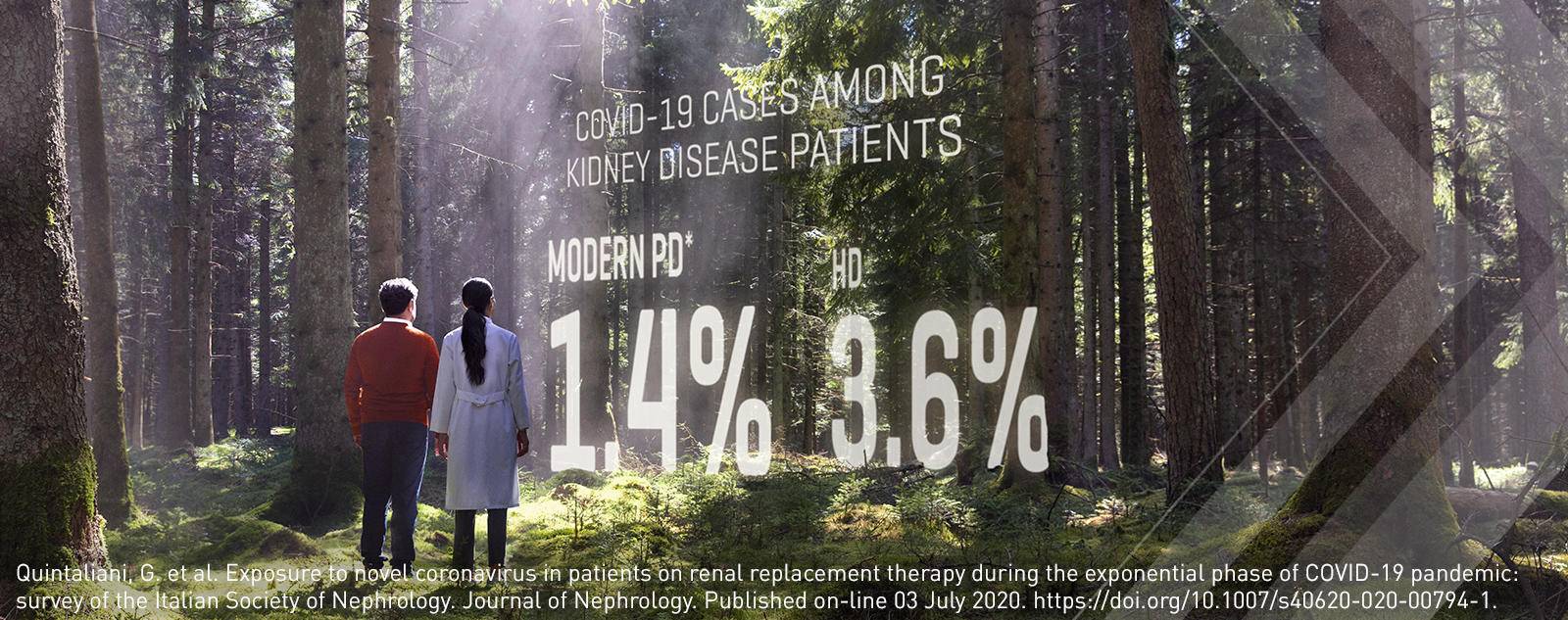
Modern PD is the safer choice for dialysis patients during the COVID-19 pandemic1
Chronic dialysis patients are among the highest-risk population for contracting and experiencing complications from viral infections. In-center hemodialysis requires patients with kidney failure to visit a dialysis clinic 2-3 times per week, putting them at significantly greater risk of contracting an infection. Modern PD therapy enables patients to receive their life-sustaining dialysis therapy in the safety of their homes.
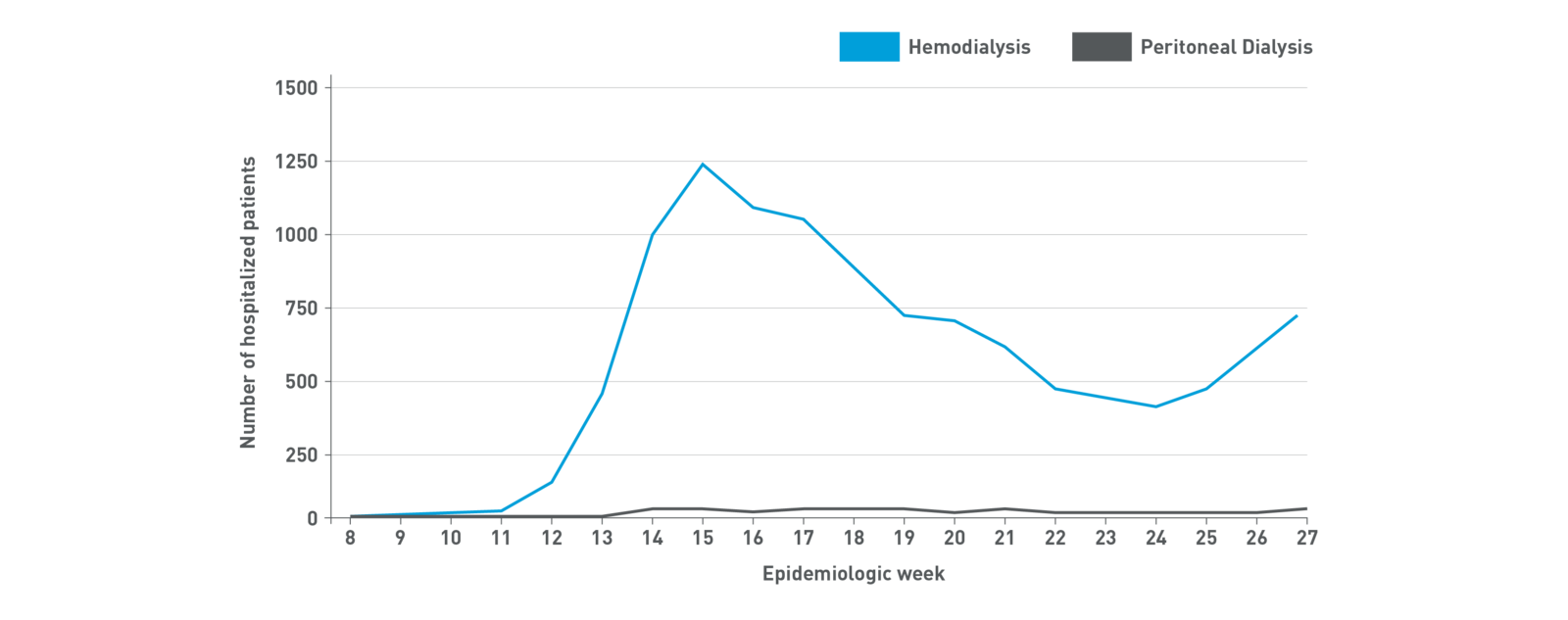
The COVID-19 hospitalization rate in the US has been consistently 3 to 4 times higher among patients undergoing HD versus PD9
The choice to reduce clinic visits
PD enables quality dialysis in the safety of patients' homes, minimizing visits to the dialysis facility and reducing the risk of exposure to viral infections.2
Patients on Modern PD visit clinics every 4-13 weeks, while patients on HD visit 156 times a year.
4-13
Visits per year on Modern PD
156
Visits per year on HD
Dialysis at home should be considered whenever possible

Professional nephrology societies have recommended that to reduce COVID-19 transmission, home dialysis be offered to all eligible patients that require chronic RRT.6-8
Home dialysis can provide life-sustaining therapy while reducing the risk of exposure to viral infections by minimizing visits to the dialysis facility.
Patients who must start dialysis during the pandemic should receive therapy at home. This includes urgent start patients.2
Consider Home dialysis first
- As the most widely used modality for home dialysis, consider PD first for both planned and urgent start patients.
- 78% of patients are medically eligible for PD.3
- Remote patient monitoring/telehealth is a safe and effective way of managing therapy without in-person visits.4
Preserve the workforce
Decreasing dialysis nurse exposure to patients with COVID-19 as a strategy to preserve the workforce.
A choice for all eligible kidney failure patients
Modern PD should be considered for all eligible kidney failure patients to help prevent nosocomial infections such as COVID-19. Modern PD is associated with a reduced risk of pneumonia, a finding that may be related to receiving dialysis at home where there is reduced exposure to infections.7
The push for home dialysis in the United States is taking on a new urgency in the backdrop of COVID-19. In the context of a pandemic, home dialysis makes even more sense. End-stage kidney disease patients are relatively immunocompromised, and the current practice of in-center dialysis does not allow for social distancing. Home dialysis can provide life-sustaining therapy while minimizing exposure.
Dr. Christopher Chan, Head of the Division of Nephrology at University Health Network in Toronto
How to implement PD during a pandemic:
- Prioritize PD for all eligible patients with kidney failure
- Ensure PD catheter placement is deemed essential surgery
- Engage and effectively deploy resources
- Use remote patient management to minimize face-to-face interaction
- Consider PD for the management of acute kidney injury in the ICU if CRRT is unavailable